An industry leader in HIV research
Paul Stoffels of Johnson & Johnson talks about the company’s broad HIV portfolio and the role of industry in advancing vaccine research.
By Kristen Jill Kresge
“At a certain point you have to jump and hope that it works,” says Paul Stoffels, vice chair of the Executive Committee and chief scientific officer at Johnson & Johnson (J&J), describing the informed risk the company is taking, with its partners, to test a novel HIV vaccine candidate in an ongoing efficacy trial. Given Stoffels’ successful career, this strategy must be working. 
After pursuing medical training in his home country of Belgium, Stoffels began his career as a young physician working in Africa. This is where he was first introduced to HIV/AIDS and its devastating consequences. He then went to work with a fellow Belgian doctor, Paul Janssen, who was the namesake of Janssen Pharmaceutica. Working together, Janssen and Stoffels began researching HIV medicines. Stoffels then became chief executive officer of Virco and chairman of Tibotec, two companies he co-founded with his business partner Rudi Pauwels. While at these companies, Stoffels and colleagues developed several antiretroviral drugs that are widely used today to treat HIV infection.
In 2002, J&J acquired Tibotec and Virco, and Stoffels joined J&J. Today, he oversees the company’s research and development pipeline and also steers their global public health strategy, which aims to make the medicines and technologies developed by the company available to the world’s poorest and most vulnerable populations. He is also credited with spurring innovation within the company by focusing on strategic partnerships, in-licensing, and acquisitions.
“Paul’s dedication to global health innovation is truly admirable, heartfelt, and deep,” says Mark Feinberg, president and CEO of IAVI. “He is a great example of how visionary and committed pharmaceutical industry leaders can make major contributions to developing biomedical innovations and new partnership models to address major public health challenges such as HIV and tuberculosis that disproportionately impact people living in low-income countries.”
The Janssen Pharmaceutical Companies of Johnson & Johnson are heavily invested in infectious disease research, including programs for HIV/AIDS, tuberculosis (TB), Ebola, polio, and respiratory syncytial virus (RSV). Their HIV portfolio includes three licensed antiretroviral drugs; a long-acting injectable antiretroviral that is being developed in partnership with GSK/ViiV Healthcare, which recently showed promise in a Phase III clinical trial; and an experimental vaccine regimen developed in collaboration with academic and U.S. government researchers that is now being tested for efficacy in a Phase IIb trial in Southern Africa (see The Imbokodo Phase IIb HIV vaccine trial, below).
Dan Barouch, director of the Center for Virology and Vaccine Research at Beth Israel Deaconess Medical Center, who helped develop and test this HIV vaccine regimen in collaboration with Janssen scientists, recognizes Stoffels’ critical role in this work. “Paul is an incredible leader of a fantastic group at Janssen. He is brilliant, passionate, insightful, and extremely effective. The HIV vaccine program would not have advanced to where it is today without Paul’s strong support,” says Barouch.
J&J also developed the first drug licensed to treat multidrug-resistant strains of TB, known as bedaquiline. I spoke with Stoffels recently, just after he returned from attending the United Nations General Assembly high-level meeting on TB, about his career, the role of partnerships in advancing infectious disease research, J&J’s HIV and TB programs, and the hope for eventually defeating this deadly duo.
How did you first become involved with HIV/AIDS?
I became involved in HIV in the early days, first as a medical student and then as a physician when I spent several years in Africa. My first time in Africa was in 1983, and then I was at a hospital in Kinshasa and I saw a lot of patients diagnosed with HIV. They were the very first patients who were diagnosed and you saw then, already, that it was a catastrophic situation. Then I lived and worked for three years in Congo and one year in Kigali, Rwanda, between 1987 and 1990. That was in the middle of the big outbreak of HIV on the African continent and where I first actually met patients with HIV and saw the challenges they faced.
Fast forward to today. How would you describe both your personal commitment and Johnson & Johnson’s commitment to tackling HIV?
Well, my personal commitment really began in my early days as a physician and that first exposure to HIV in Africa. Since then I’ve worked with HIV pretty constantly throughout my career. I worked with Dr. Janssen first in the early 1990s on new molecular drug designs for HIV and then I left the company to start my own companies, Tibotec and Virco, with Rudi Pauwels, my business partner. These two companies discovered and developed a few HIV medicines and then they were acquired by Johnson & Johnson, at which time I joined J&J, leading their HIV program.
J&J and Janssen have three main HIV drugs: Prezista, which is a protease inhibitor also known as darunavir; the non-nucleoside reverse transcriptase inhibitor [NNRTI] Intelence, also known as etravirine; and the second-generation NNRTI Edurant, which is also called rilpivirine. All three medicines were developed initially at Tibotec and are now used in first-line, second-line, and third-line treatment regimens in combination with other drugs. So we still have a very active business and are also active in HIV research, including a vaccine candidate that is now being tested in an efficacy trial in Africa.
Part of your role at J&J is steering the global public health strategy. What does that strategy entail and how do you view this component of your work?
If you want to implement programs to treat diseases like HIV and TB, you have to have people on the ground to help with training and implementation. These things don’t happen automatically with new drugs, especially if you have complicated medicines, like second-line therapies for HIV. So we set up our global public health team to be fully dedicated to developing and ultimately supporting access to medicines and devices that have an important impact in the developing world. Right now we have about a hundred people on our global public health team—including colleagues in Africa and Asia, who work with the local companies we have in the countries.
There are four key global public health priorities we are tackling at the moment. One is in the availability of our HIV drugs, which we deploy in Africa through generic companies, or directly ourselves. We also have a big program in TB, through which we are bringing bedaquiline to treat multidrug-resistant TB in all countries that have a high need, and the vast majority of those are in the developing world. Then we have a mental health program to evaluate whether new long-acting antipsychotics can be helpful in treating patients on the African continent. Finally, we are working to lessen the burden of intestinal worms in children through our mebendazole donation program.
We also have a collaboration between our global public health and vaccine programs to conduct clinical trials. As we speak, we have 11 clinical trials running around the world, some of which are in Africa. We have an HIV vaccine that is being tested in Southern Africa, and we also have clinical trials ongoing for new vaccines against Ebola, Zika, polio, respiratory syncytial virus (RSV), and drug-resistant forms of the bacteria E. coli.
You mentioned the ongoing Phase IIb HIV vaccine trial. J&J is also involved in development of the vaginal ring containing the antiretroviral dapivirine. What role do you think pharmaceutical companies should have in HIV prevention research, particularly in vaccine research and development?
I have been doing drug and vaccine development for 25 years and I believe that industry has the platforms, resources, and capabilities needed to translate innovative ideas and basic science into solutions for people in need. However, at the same time, research and development can be a slow, long process, and you may never get to an approved product. So there have to be collaborations and partnerships between the public sector, not-for-profits, and industry to keep the momentum going.
At J&J we have about 10,000 people in R&D, so we have all kinds of capabilities to deploy, whether it’s statistics, clinical trials, pharmacology, vaccine platforms, antibody knowhow, or developing long-acting formulations. All these technologies and platforms can be used for both treatment and prevention.
For HIV, we had to first understand the science and then develop new medicines. The vaginal ring is an application in development to deliver one of these medicines. Our long-acting technologies were originally developed for schizophrenia and now we are working to apply those learnings and make a long-acting injectable for HIV treatment containing two antiretrovirals, one of which is rilpivirine. We now have two Phase III studies together with GSK that showed very good results and I think it’s going to get to market as a monthly injection for HIV treatment.
And for all of this, we have collaborated with others. The development of our TB drug bedaquiline was done in collaboration with the TB Alliance, the vaginal ring with the International Partnership for Microbicides [IPM], and our HIV vaccine clinical trials have been conducted in collaboration with several partners, including the Bill & Melinda Gates Foundation; the National Institute of Allergy and Infectious Diseases [NIAID], part of the U.S. National Institutes of Health [NIH]; the U.S. Military HIV Research Program at the Walter Reed Army Institute of Research; Beth Israel Deaconess Medical Center; the Ragon Institute; the NIAID-funded HIV Vaccine Trials Network; the South African Medical Research Council; and the International AIDS Vaccine Initiative. So it’s all the result of different types of collaborations.
Even the development of the mosaic HIV vaccine candidate seems to have been a uniquely collaborative process between Janssen and Dan Barouch. Was it?
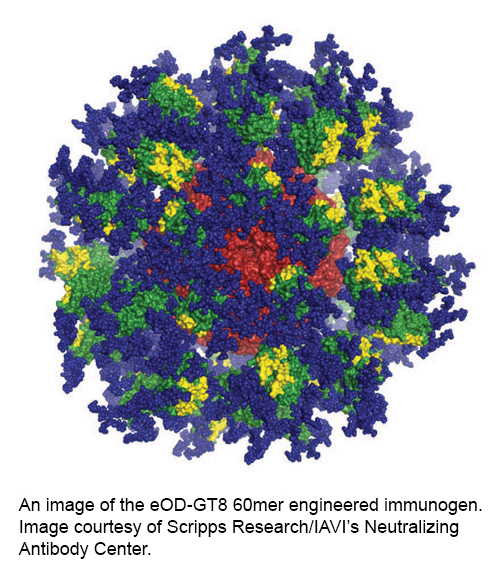
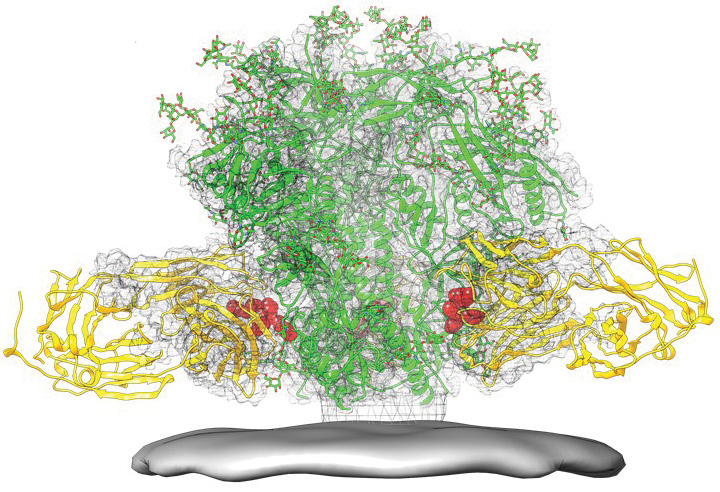
I don’t know whether it is a unique collaboration, but I don’t know many others like it. In this case, we were able to bring together our biological capabilities with Dan Barouch’s scientific work with animal models and laboratory work in non-human primates, which was done in collaboration with researchers at the U.S. Military HIV Research Program. The mosaic immunogens incorporated in the vaccine were designed by the Los Alamos National Laboratory. It was a very integrated partnership, built first on the scientific and medical capabilities of the different groups, with a long-term commitment to get to a solution and in the end develop a product. All the time we worked on scaling up and validating the product, making the different vaccine constructs, and are now testing them for efficacy in people with support from the Bill & Melinda Gates Foundation and the NIH.
And are you optimistic about the prospects for the candidate given the preclinical data?
Yes. We wouldn’t be in the clinic if we weren’t. And it’s not just us—our partners are also optimistic, which is why we have joined forces to evaluate this vaccine candidate in a large-scale clinical trial. Based on the animal models and the experience with the RV144 trial, which was the first trial to show some kind of efficacy, I think we should see something. Something significant. You never know with an HIV vaccine, but you have to test it before you can even predict what it’s going to do. It could completely fail, but at a certain point you have to jump and hope that it works.
Something else that the HIV field seems to be grappling with these days, particularly with respect to oral pre-exposure prophylaxis [PrEP], is the need to think about access and implementation earlier on in the development process so that once a product is developed there isn’t as much of a lag time between product licensure and introduction in developing countries. How do you think about these issues at J&J with regard to the eventual access and affordability of the HIV prevention products you are developing?
We have a very strong mission in that regard. You don’t start this type of work without knowing that you have to make this available to people in countries where health care spending amounts to a few dollars per person per year. We commit to access, jointly with our partners, meaning any HIV prevention product has to be accessible on a large scale. So we carefully consider a pricing strategy that takes the economic status of different countries into account. For TB products, which only have a developing world market, it is very difficult to offset your investment in innovation and it can be a challenging business model for companies.
And what about issues of acceptability by the ultimate recipients of these products, particularly for a product like the dapivirine vaginal ring that requires regular use to be effective? Is this something you and your colleagues are thinking about?
With the ring, yes. I think IPM’s decision to go from a vaginal gel to a once-monthly ring was extensively tested and evaluated for feasibility and it was found to be the best possible option.
For an HIV vaccine, our approach is to just get to maximum possible efficacy, which right now requires four injections over the course of a 12-month period. And that is where, for me, acceptability is not the first question. The first question is: Can we get it done? Can we protect people from HIV? Then, the second question is: Is it feasible to have four injections in a year?
But I think you have to say that if there is more than a 50 percent chance that this vaccine will protect you from HIV, to be very conservative, then I don’t think four injections is such a burden. Acceptability comes in as a second phase. It all has to do with the level of efficacy. If this is highly efficacious, people will use it.
What is the one message you think is important in the conversation about HIV today?
The world should stop saying that HIV is over. It’s not over. It is still a huge challenge and we shouldn’t get too optimistic. The HIV epidemic is only at the beginning. It is fantastic how many people are on therapy, but it is also a huge challenge to keep them on therapy for the next several decades. People who are infected will need to be on therapy for 40 years to live a normal life and that comes at a huge cost.
Also, we are not going to stop the spread of HIV in the near future without a vaccine or other good prevention tools. This could be a combination of PrEP, a vaginal ring, long-acting injectables, but the bottom line is we need many prevention tools, as well as better therapies to address the need for long-term use.
You just returned from the U.N. high-level meeting on TB. Was there renewed optimism for TB vaccines there following the recently reported clinical data?
Yes. The meeting was highly attended by many ministers of health from all over the world and some heads of state, so it was quite impressive, and the vaccine data is great because we will never end the epidemic without a vaccine. But it will take some time before we’re there.
Is J&J currently involved in TB vaccine research?
No, not at the moment. We had some TB vaccine activity that didn’t work out, but we are working on developing TB drugs. We have the first new TB drug in over 40 years, bedaquiline, which we developed over 15 years and is now being implemented with fantastic success for patients. So that’s a good first step. We also have four new targets that we discovered and are working on to get to new drug combinations, so we are still very active in TB research with our partners. We have collaborations with the Institute of Microbial Technology in India, and with many partners around the world to develop new TB drugs.
| Renewed promise for tuberculosis vaccines |
|
Two recent studies are injecting promise into the decades-long quest to develop newer and better vaccines against tuberculosis (TB), the world’s deadliest infectious disease and the top killer of people who are living with HIV. In July, a Phase II trial showed that revaccinating South African adolescents with the only licensed TB vaccine, known as BCG (bacille Calmette-Guérin), that they received as infants was 45 percent effective in preventing sustained TB infection (N. Engl. J. Med. 2018; 379:138-149). The BCG vaccine was developed nearly 100 years ago and is administered routinely to infants in high-incidence settings to protect against the development of TB disease; however, its efficacy is variable and the precise duration of the protection it affords is unknown. Revaccination might be a viable way to extend the protection of the BCG vaccine into adolescence. Then in September, results from a Phase IIb study involving more than 3,500 adult volunteers from Kenya, South Africa, and Zambia showed that GSK’s investigational TB vaccine candidate known as M72, administered along with the company’s AS01E adjuvant, was 54 percent effective at preventing active pulmonary TB disease from developing in adults with latent TB infection (DOI: 10.1056/NEJMoa1803484). These scientific advances come at a time when TB is also receiving increased political attention. Researchers are now hopeful that political will, funding, and scientific progress will come together to help reduce the global TB disease burden, which remains staggeringly high. In 2017, there were 10 million new cases of TB disease reported according to the World Health Organization. |